By Michelle Strange, MSDH, RDH
If I have heard it once, I have heard it a thousand times; We load the autoclave like this! *Inserts items the wrong way*. That’s how you did it with the last autoclave? That’s great, but what makes you think this one is the same?
The correct answer is; what do your instructions for use say? Not all autoclaves are made equal, and if you haven’t gotten to know yours, you could be misusing it and putting your patients at risk. However, you can apply some general rules to most autoclaves to set them up for sanitization success!
Dos
- Follow The correct answer is; what do your instructions for use say? Not all autoclaves are made equal, and if you haven’t gotten to know yours, you could be misusing it and putting your patients at risk. However, you can apply some general rules to most autoclaves to set them up for sanitization success!

- Make sure instruments undergone cleaning and disinfection, prior to sterilization. International guidelines state that the entire process of instrument reprocessing needs to be performed by trained personnel using monitored procedures to ensure reproducibility. These requirements contribute to the health and safety of patients, users and third persons.

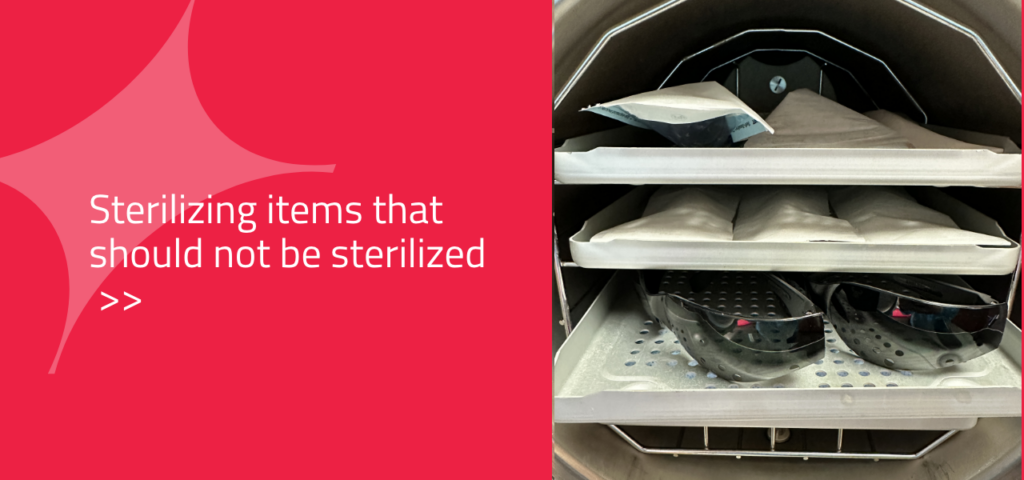
- Ensure you only put items in the autoclave that can withstand the high temperature and pressure required for sterilization, such as glass, metal, and plastic instruments.
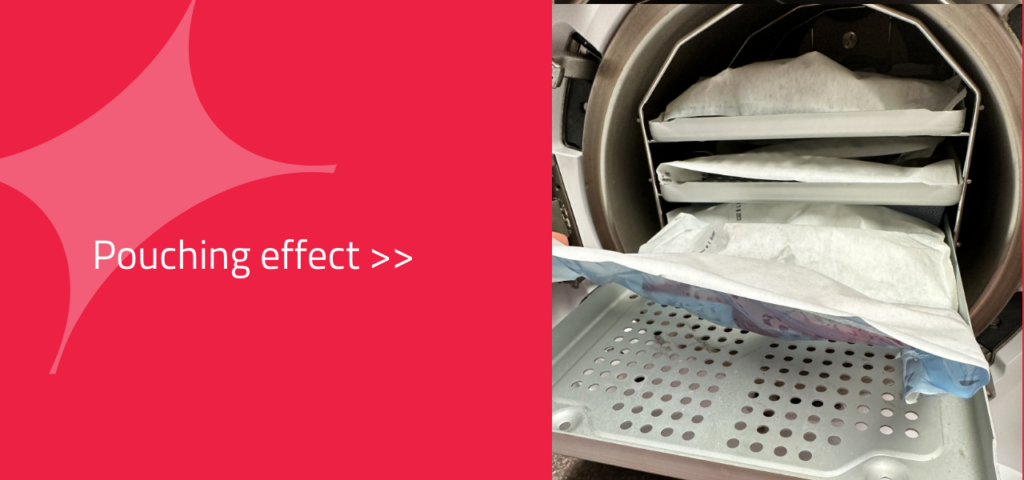
- Arrange the items in a way that allows for efficient steam penetration and circulation. Items should not be tightly packed, and there should be space between them. Be aware of the “pouching effect,” which can occur if objects are placed too close together in the autoclave.
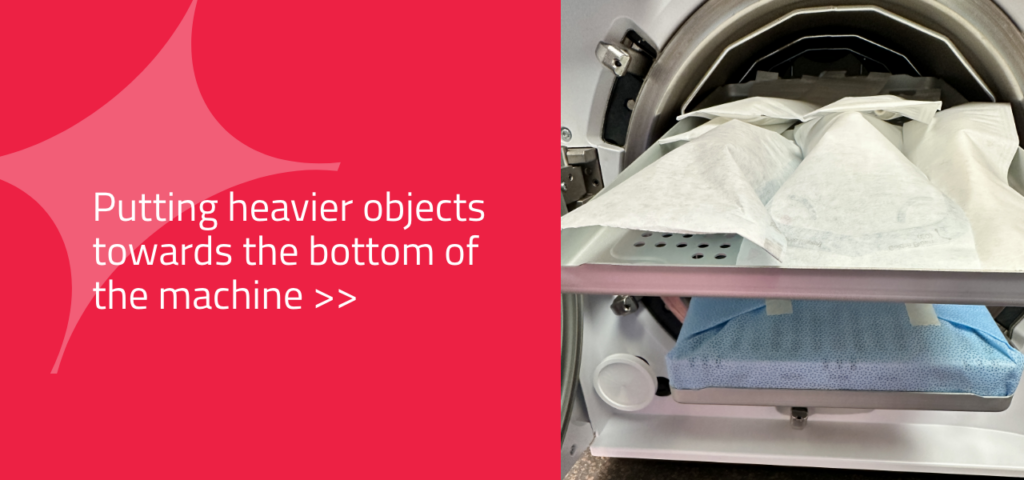
- Place heavier items on the bottom of the autoclave and lighter items on top to ensure that steam reaches all items. Or use racks to place cassettes on their sides to maximize the steam penetration.
- Run your autoclave! What I mean is, even if it isn’t completely full, go ahead and run it. In busy practices, we often wait to fully load the autoclave, then we try to get every last instrument that is wrapped and ready to go inside the chamber for that load. This often leads to it being overloaded. It is ok to load your autoclave and run it before it is completely full.

- Use a chemical / biological indicator to receive an immediate indication of the quality of the sterilization.

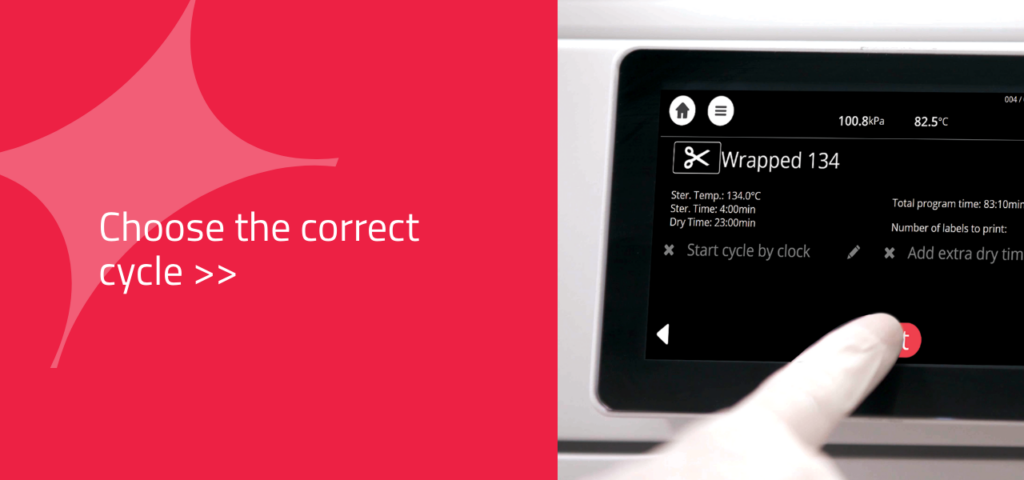
- Apart from loading the autoclave correctly it is also very important that the customer is choosing the correct cycle. This means, the right temperature, wrapped or unwrapped makes a big difference and, in some cases, the prion cycle might be needed.
- Keeping the autoclave clean!! It is contradictory to render ‘sterile’ instruments from a device that is very dirty.

- Check the cycle result and then approve and document the cycles.

Don’ts
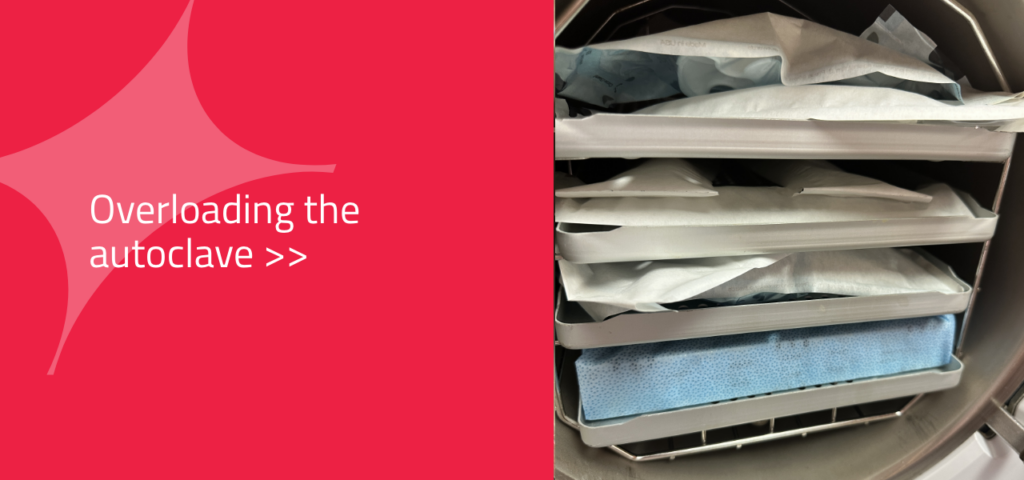
- Do not overload the autoclave. Overloading can prevent steam from circulating properly around the materials, resulting in ineffective sterilization. This happens so easily in a busy practice or if you are running behind and have many instruments to sterilize, and they often just get shoved in willy-nilly. Don’t do it! You are increasing your risk of infection significantly
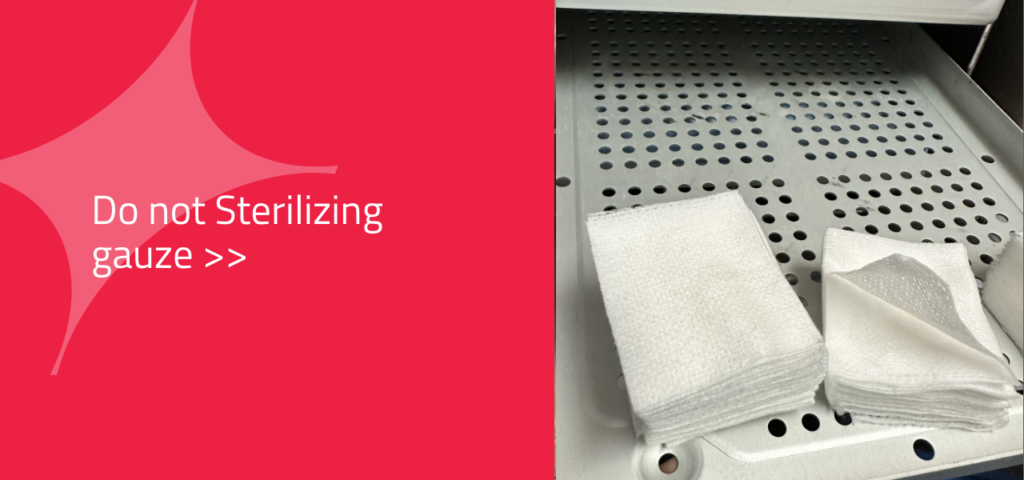
- Do not use packaging that isn’t designed for use in an autoclave. Using improper wraps or pouches, sometimes even gauze, can lead to breakage or malfunction, which can be hazardous.
- Do not place materials that cannot withstand high temperatures or pressure inside an autoclave, such as paper towels, cloths, or rubber gloves. These will be damaged by heat or steam during the sterilization process and possibly result in the contamination of objects inside the chamber.

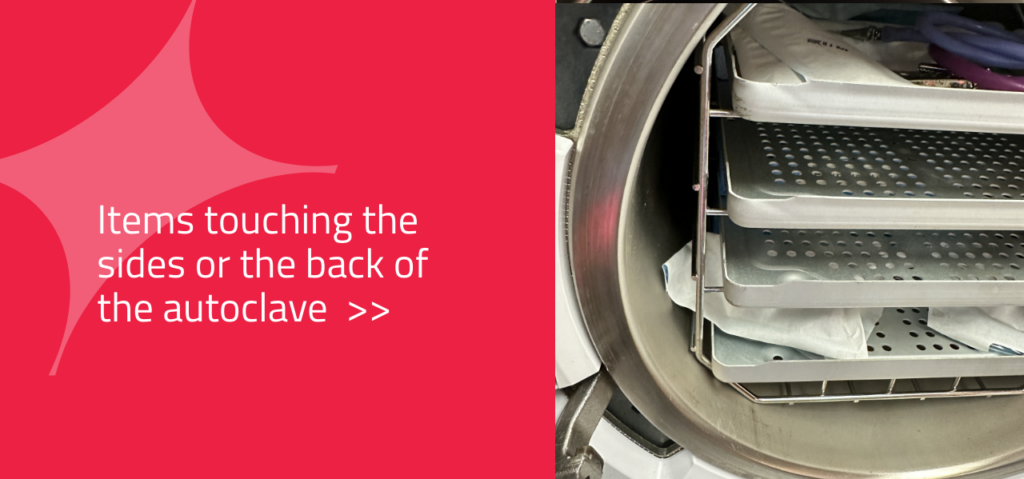
- Do not place items too close to the walls of the chamber, or door of the autoclave, as this can interfere with steam circulation and lead to incomplete sterilization.
- Do not be afraid to remove a tray from the chamber so larger cassettes have room and can have sufficient steam reach its contents.

Train your staff regularly!
Regular training for autoclave use in dental practices is critical. Without regular training on proper autoclave use, staff may be using outdated techniques that are ineffective in sterilizing instruments, leading to potential risks of cross-contamination and patient illness.
By ensuring staff members remain educated on the latest developments in autoclave use, dental practices can guarantee their patients receive the highest quality of care possible.
GUEST AUTHOR
Michelle Strange, MSDH, RDH
Michelle Strange, MSDH, RDH, brings over 20 years of experience to her numerous roles in dentistry. A graduate of the Medical University of South Carolina with a Bachelor of Health Science and the University of Bridgeport with a Master’s in Dental Hygiene Education, she focuses her career on expanding the knowledge of her colleagues in all aspects of health care. Her passion for dentistry and its connection to overall health extends to her community and global efforts. Michelle was the co-founder of the longest-running podcast for dental hygienists, A Tale of Two Hygienists.


